Urinary tract infections can often lead to symptoms like painful urination and general discomfort, affecting countless individuals each year.
UTIs represent a notable portion of primary care consultations – accounting for approximately 1–3% – and they are responsible for about 14% of all antibiotic prescriptions in community healthcare settings in the UK.
I’ve observed that at least half of the female population is likely to experience a UTI at some point in their lives, with many suffering from recurrent episodes. This high incidence rate highlights the need for increased awareness and effective management strategies for UTIs.
Also, it is worth to know that regulating microbes is possible through the consumption of probiotics.
Today, I’d like to present my two cents on:
- Urinary Tract Infections are common, affecting a significant portion of the population globally.
- Women are more susceptible to UTIs due to their anatomical structure, with at least half experiencing a UTI at some point in their lives, often facing recurrent episodes.
- The gut, vaginal, and urinary microbiomes play crucial roles in the development and prevention of UTIs.
- Uropathogenic E. coli, normally part of the gut flora, can cause UTIs when it migrates to the urinary tract.
The Gut and Urinary Bacteria
The complex relationship between gut microbiota and Urinary Tract Infections (UTIs) is crucial in addressing these widespread infections. The human gut has a diverse range of bacteria, playing a vital role in maintaining overall health and preventing diseases.
Among these microorganisms, specific strains like uropathogenic E. coli (UPEC) are known for triggering UTIs. Normally harmless as part of the gut flora, these bacteria become a concern when they travel to the urinary tract.
| Factor | Impact on UTIs |
|---|---|
| UPEC Presence | Increases UTI Risk |
| Anatomical Proximity | Facilitates Bacterial Migration |
| Antibiotic Use | Disrupts Microbial Balance |
| Dietary/Stress Changes | Leads to Dysbiosis |
While antibiotics are crucial for treating various infections, they can accidentally cause damage to the gut microbiota. That is why they are usually not consumed together with probiotics.
These medications often eliminate both harmful and beneficial bacteria, diminishing the diversity of microbes in the gut. The significance of a healthy gut microbiome goes beyond UTI prevention. A well-balanced gut microbiota is essential for effective immune function, nutrient absorption, and mental health.
Thus, maintaining gut health is a key preventive strategy against UTIs and a fundamental aspect of overall wellness. It is in close connection with mental health as well, especially when treated with probiotics.
| Strategy | Benefit |
|---|---|
| Balanced Diet | Promotes Diverse Microbiota |
| Controlled Antibiotic Use | Prevents Microbial Imbalance |
| Probiotic Intake | Restores Beneficial Bacteria |
| Stress Management | Reduces Risk of Dysbiosis |
Recurrent UTIs and Microbial Resistance
Recurrent UTIs (rUTIs) pose a significant challenge, particularly for women. The frequent use of antibiotics for UTI treatment not only leads to antimicrobial resistance (AMR) but also disrupts the natural microbial balance in the body. This disruption can make women more susceptible to further infections.
The development of non-antibiotic strategies, such as the use of probiotics for women, is crucial in managing rUTIs. Probiotics, by restoring and maintaining a healthy microbial balance, can reduce the recurrence of UTIs and mitigate the risk of AMR. Not to mention that probiotics can be of use during pregnancy.
The Urinary Microbiome
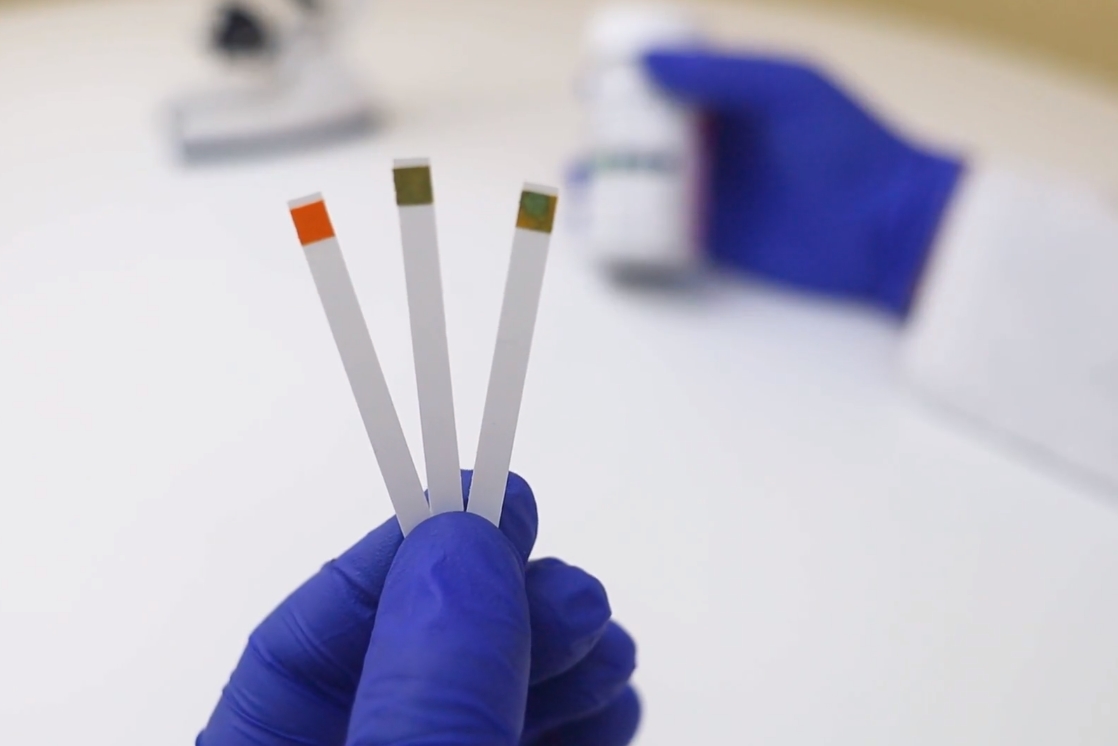
The urinary microbiome has revolutionized the understanding of urinary health and Urinary Tract Infections (UTIs). Contrary to previous beliefs that urine is sterile, it is now known to host a complex array of microorganisms.
This microbiome plays a crucial role in maintaining urinary tract health and preventing infections.
- The urinary microbiome is composed of various bacteria, including beneficial strains that help maintain the urinary tract’s health.
- A diverse and balanced urinary microbiome acts as a natural barrier against infections.
- Factors such as antibiotic use, hormonal changes, dehydration, and certain health conditions can disrupt this delicate balance.
- Understanding the role of the urinary microbiome has led to new approaches in UTI prevention and treatment.
- Probiotics, particularly those targeting urinary health, are being explored as a means to support or restore the urinary microbiome.
- Ongoing research is focused on identifying specific strains within the urinary microbiome that play key roles in preventing UTIs.
The Vaginal Microbiome
The vaginal microbiome is a key player in the urinary tract’s health, exerting a significant influence on the risk and recurrence of Urinary Tract Infections (UTIs). In a healthy state, the vaginal flora is predominantly composed of Lactobacilli species.
These beneficial bacteria are instrumental in maintaining an acidic environment in the vagina, which is inhospitable to pathogenic organisms. This acidic milieu is crucial for inhibiting the growth and colonization of uropathogenic bacteria, such as E. coli, which are common culprits in UTIs.
By doing so, Lactobacilli serve as a natural defense mechanism, significantly lowering the risk of developing UTIs. The delicate balance of the vaginal microbiome can be easily disrupted, leading to a condition known as dysbiosis. Factors contributing to this imbalance include antibiotic use, hormonal changes, stress, and certain hygiene practices.
A decrease in Lactobacilli levels, in particular, can make the vaginal environment more conducive to the growth of harmful bacteria. This shift in the microbes not only increases the vulnerability to UTIs but can also lead to other complications like bacterial vaginosis and yeast infections.
The importance of Lactobacilli in preventing UTIs has brought probiotics, especially beneficial for women, into the spotlight. Probiotics containing Lactobacilli strains are increasingly recognized for their role in restoring and maintaining a healthy vaginal microbiome.
By supplementing the natural flora of the vagina with these beneficial bacteria, probiotics can help re-establish the acidic environment, thereby reducing the likelihood of pathogenic bacteria thriving and causing infections.
Alternative Treatment Strategies
The increasing prevalence of antibiotic resistance and the adverse effects associated with prolonged antibiotic use have necessitated the exploration of alternative treatment strategies for Urinary Tract Infections (UTIs).
Probiotics, especially probiotics for women, have gained significant attention. These probiotics are emerging as a viable option for managing urinary health.
Mechanism of Action
Probiotics function by promoting the growth of beneficial bacteria in both the vaginal and the gut microbiome. This enhancement of healthy bacteria helps in establishing a natural defense mechanism against pathogenic bacteria responsible for UTIs.
Protective Barrier
By reinforcing the beneficial bacterial population in the gut and vagina, probiotics create a protective barrier. This barrier reduces the likelihood of harmful bacteria gaining a foothold and causing UTIs.
Safety and Cost-Effectiveness
One of the key advantages of probiotics is their safety profile. They are generally well-tolerated with minimal side effects, making them suitable for long-term use. Additionally, compared to the ongoing costs and potential health impacts of recurrent antibiotic treatments, probiotics are a cost-effective solution.
Prevention of Recurrent UTIs (rUTIs)
For women who suffer from recurrent UTIs, probiotics offer a preventive strategy. Regular intake of probiotics can help in maintaining a balanced microbial environment, thus reducing the frequency of UTI episodes.
Complementary Approach
Probiotics can be used in conjunction with other lifestyle modifications for a more comprehensive approach to UTI prevention. This includes adequate hydration, dietary changes, and proper hygiene practices.
Emerging Research and Customization
Ongoing research is focusing on identifying specific probiotic strains that are most effective in preventing UTIs. This could lead to the development of customized probiotic formulations tailored to individual needs.
FAQs
What is the pathogenesis of a urinary tract infection?
The pathogenesis of a UTI involves bacteria entering the urinary tract, adhering to the urothelium, and triggering an immune response. This results in inflammation and typical UTI symptoms.
What is the pathophysiology of a urinary tract infection?
In the pathophysiology of a UTI, bacterial invasion causes inflammation of the urinary tract lining, leading to symptoms like pain, burning during urination, and increased frequency and urgency of urination.
Is urinary tract infection a virus, bacteria, or fungi?
UTIs are most commonly caused by bacteria. While less common, fungi and viruses can also cause UTIs, but bacterial infections are the predominant cause.
What kills E. coli in the urinary tract?
Antibiotics are the primary treatment for killing E. coli in the urinary tract. Commonly prescribed antibiotics include trimethoprim/sulfamethoxazole, nitrofurantoin, and ciprofloxacin.
Summary
I’ve increasingly turned to probiotics as a viable, cost-effective, and safe alternative to traditional antibiotic treatments for UTIs. The growing body of research consistently supports the benefits of probiotics in preventing UTIs.
This evidence positions probiotics as a promising tool in our ongoing efforts to combat these infections, offering a preventive approach that aligns with the body’s natural systems.